Opiate
Opiate, a powerful drug, raises levels of pleasure chemicals in the user’s brain. The flood of chemicals causes extreme pleasure, calmness and suppresses appetite. The drug relaxes some people and energizes others. Repeated drug use causes the brain to adapt to the higher levels of chemicals. As a result, the user gets agitated, depressed and uncomfortable when they don’t have the drug. Signs of opiate use include nausea, constipation, vomiting and being sleepy. Users most commonly snort, inject or smoke opiate.
Opiate use disorder and addiction
Regular use of opiate usually causes severe addiction. Addicts usually take the drug in larger amounts and for longer periods of time than they intend; wanting to cut down or quit the drug but not being able to; spending a lot of time obtaining the drug; craving or a strong desire to use the drug; repeatedly unable to carry out responsibilities at work, school, or home due to opiate use; continuing use of the drug despite social problems caused or made worse by use; stopping or reducing important social, work, or fun activities due to using.
Recurrent use of the drug in physically hazardous situations is also a sign of addiction; consistent use of the drug despite knowledge of physical or psychological difficulties from using; physical tolerance as defined by a need for increasing amounts of the drug to achieve intoxication or less effect with continuing use of the drug; and physical withdrawal symptoms or substance use to avoid withdrawal.
Treatment of opiate use disorder and addiction
Moderate to severe opiate use disorder and opiate addiction usually requires medical detoxification and inpatient treatment in the beginning at a partner facility. Accordingly, inpatient treatment separates the user from the drug and related stressors and triggers. After initial medical detoxification and inpatient stabilization, levels of care for continued treatment are assessed with six dimensions:
- Acute intoxication or withdrawal potential
- Biomedical conditions and complications
- Emotional, behavioral, or cognitive conditions and complications
- Readiness to change
- Relapse/continued use, continued problem potential
- Recovery environment
Based on the severity of the opiate use disorder AND the findings of the 6-dimension assessment, experts recommend treatment based on levels of care:
- Inpatient
- Residential
- Outpatient
- Follow-up
Experts recommend extended programs life-skills, coping-skills, dual-disorders and “sober housing” to augment basic treatment. Research shows that the best long term results, when treating opiate addiction occur by starting with a minimum of 90-days of intensive/primary treatment, before reducing intensity. Afterward, experts usually recommend structured recovery-support for two years, while the brain continues to recover and restore normal functioning.
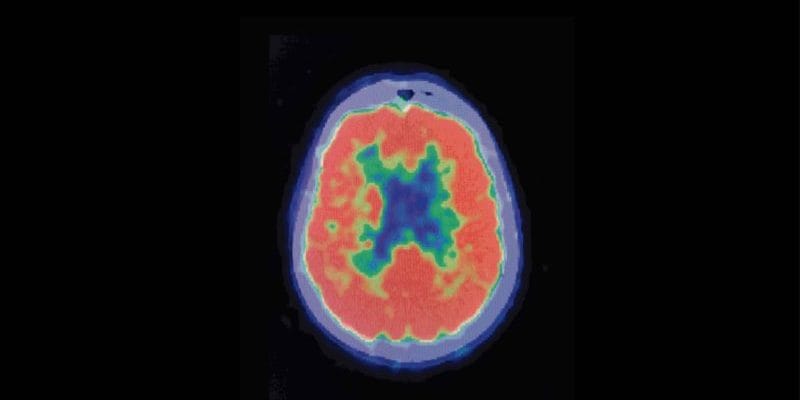
Understanding dopamine and how the brain gets “hijacked” by addiction
Do you know what is like to be distracted by something so much that it was hard for you to stop looking at it? Pre-occupied with hunger and unable to focus on anything but your growling stomach? Stuck in your thoughts about a relationship? Ever just want to “change the channel” but you couldn’t? Yes? Multiply that feeling by 10 or 100. Opiate addiction is like that, it “hijacks” the reward center of the brain. Think of it this way, eating a meal or being with someone you love feels good, right? Well, just imagine that good feeling . . . now multiply it times 10 . . . now times 100. Imagine how great that would feel.
That’s what using opiate can feel like to an addicted person. Using the drug elicits extreme and temporary pleasure. It also elicits extreme and lasting mental pre-occupation.
For a opiate addict, the pursuit of that pleasure becomes all-consuming. As a result, pleasure-chemicals supercharge certain brain connections, while the connections between good judgement and behavior become much weaker.
The Defensive Brain
As addiction takes hold, the thinking part of the brain gets pre-occupied with obtaining the “super-pleasure” provided by the drug. The addicted brain responds to the idea of cutting back or quitting the drug as a threat to survival. The using brain quickly dismisses the idea, rationalizing and justifying reasons for continued use. The brain crafts excuses, making continued drug use seem like the right thing to do. Addicts still think. It is just that the thinking and problem-solving part of the addict’s brain becomes more and more driven to figure out how to keep using the drug, no matter what. Eventually, the obsession with using takes over all the brain’s resources.
Conclusion
Trying to quit opiate FEELS like deprivation of food or ending an important relationship. Without proper treatment, structure and support, most people relapse. The pursuit of the “super-pleasure” is all-consuming. Regular opiate use changes the brain’s chemistry and structure. But with the right treatment and follow-up, normal brain-function will be restored over time. With rigorous treatment, diligent follow-up and supportive monitoring, lasting recovery becomes possible.